A brief look at vaccine development and research.
As I write this, in early May 2021, there have been more than 170 million COVID-19 cases and 3.7 million related deaths; and numbers are expected to rise. In time of crisis, it is helpful for us to look back at humanity’s past success in eradicating a devastating illness using science. We are talking about how we officially eradicated the infection called Polio.
Polio has been around since prehistoric times as an endemic pathogen. At the beginning of the twentieth century, there were frequent epidemics in the Americas and Europe, and later around the world. At its peak half a million people died or were paralysed worldwide each year.
Box 1: FAQs about Polio
After living through a pandemic, we know what are the important questions to ask about any virus.
- What is it? Polio, short for poliomyelitis, is an infection caused by the poliovirus.
- What does it do? It can affect the nervous system. Severe infections leave muscles permanently damaged, resulting in paralysis. In rare cases, it could disable brain function for breathing resulting in death. Most of the infections do not result in illness. But about 1% of cases would lead to paralysis.
- How does it spread? After the first exposure, the incubation period is 6-20 days for symptoms. For several weeks, the virus is excreted via faeces. It is highly contagious via faecal-oral and oral-oral routes, meaning it can be transmitted through poor hygiene and contaminated food and water.
- Are there any risk factors for polio? Children, immune deficiency, malnutrition, and pregnancy.
- Is there any cure? No treatment will cure polio. Only extensive care with rest and good nutrition can alleviate some symptoms.
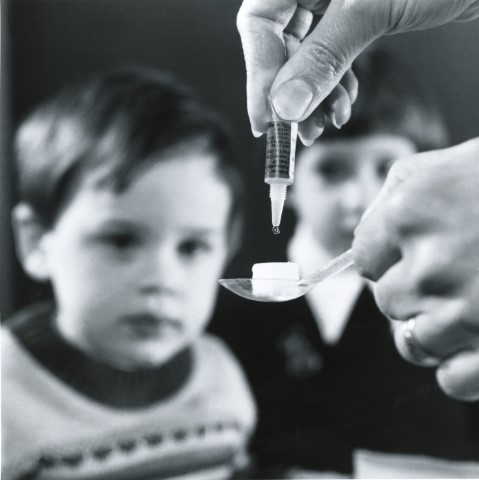
- Is there any vaccine? Yes! There are two kinds of vaccines. Remember, Amitabh Bachchan appearing on TV and radio “Do Boond Zindagi Ki” during the Pulse Polio campaign.
Box 2: The Working Principle of Vaccination
There are germs all around us, and we are susceptible to encountering these pathogens, which are disease-causing organisms. Our body usually does an excellent job at defending us from them by having physical barriers like hair, skin, and mucus. Even if some pathogen succeeds in infecting us, our immune system is triggered. Each pathogen like a virus or bacterium is made up of a lot of parts, one of these parts is called an antigen. This part activates the immune system to produce antibodies. One can imagine antibodies act as soldiers that fight the pathogen of a specific antigen. We have a lot of distinct types of antibodies, soldiers trained for different but specific antigens. On encountering an infection, our immune system starts ramping up the production of antibodies and overcomes the pathogen. These antibodies also produce memory immune cells which remain alive even after defeating the infection. If the infection recurs happens the memory cells are ready to produce antibodies. But sometimes there are not enough antibodies produced causing pathogens to overpower the immune system leading person falling ill. Vaccination is used to train your immune system against specific dangerous pathogens. Vaccines have a weakened or inactive part of the pathogen (antigen) which provokes an immune response to produce antibodies and memory cells. Thus, the body is ready to fight that disease in the future. This way world has been able to stop many dangerous diseases like smallpox, measles, and polio.
Early scientific discoveries leading to the polio vaccine
Vaccine development as scientific progress happens through a series of steps, where collective knowledge of humanity is integrated and developed to push research further. Polio vaccine development is the same. In 1894, the first Polio outbreak was discovered in the US, where 132 cases of paralysis were detected. Charles Caverly, a physician there, identified it as an acute nervous system disease which may or may not result in paralysis. It was in 1905 that the series of outbreaks in Sweden led Ivar Wickman to report the contagious nature of polio and asymptomatic disease carriers. This information was critical for people to use personal hygiene for children as a preventive measure against the Polio contagion and opened research into isolating the infecting agent of the contagion, i.e., the virus. Karl Landsteiner and Erwin Popper from Vienna were the first to call polio a virus. They filtered the spinal cord fluid from people infected with polio to isolate the virus. They could artificially develop polio in monkeys using filtered poliovirus. During this time, summer polio epidemics became common causing lockdowns of public spaces for children. Researchers solving this problem realized that there was more than one type of poliovirus. In Australia, Frank Burnet and Jean Macnamara used monkeys to test various polioviruses and see that the immunity to one type did not provide protection.
Polio vaccine: live and killed vaccine
In the twentieth century, there were two major kinds of vaccines: one was the inactivated vaccine (killed vaccine), and the other was the attenuated vaccine (live vaccine). The inactivated vaccine contains parts of the killed pathogen that will incite an immune response similar to that provoked by the live virus but without the terrible consequences. The virus is usually killed by heat or formaldehyde. On the other hand, an attenuated vaccine contains a live virus, whose virulence is reduced while keeping it alive. Virulence is reduced when a virus is allowed to replicate in a live host, classically a chicken egg, within a lab environment till it evolves into an innocuous version of itself.
In 1935, two American teams were working on vaccine trials with the two different kinds of vaccines. One John Kolmer working with live vaccine conducted trials on 10000 children, which did not go well. Five children from the trial died and ten were paralyzed. He made the mistake of having no control group, a group that is given a placebo, leading to mistrust of the reports. This failure led to Kolmer being called a murderer. At the same time, Maurice Brodie’s killed-virus vaccine trial results showed 1 in 7500 people given the vaccine got polio and in the control group, 5 in 4500 got it. These results were promising but the difference between the control group and the vaccinated group was not statistically significant. Amid safety issues of the Kolmer vaccine and cancellation of his project, Brodie’s vaccine was declared ineffective; the whole vaccine project was hastily scrapped, and Brodie was fired from the New York City Health Department. Many researchers say that the hasty cancellation of these projects pushed the vaccine trials back 20 years.
Albert Sabin and Jonas Salk vaccine
Anyhow, the next year 1936 in New York City Albert Sabin and Peter Olitsky found out a new technique to cultivate poliovirus in human embryonic brain tissue. This vaccine would have risks as it would affect the recipient’s nervous system. Sabin continued to elucidate the basic functioning of the virus. In 1941, the common conception was that the virus is only in the nervous system. Sabin along with Robert Ward challenged this and discovered the poliovirus in the digestive system.
Working and testing animals like monkeys was time-consuming and frustrating for many researchers. To solve this issue breakthrough in culturing viruses was required, and this breakthrough came in 1949. The team of John Enders from Boston successfully cultured the poliovirus in human embryonic skin and muscle tissues. This would make producing massive quantities of viruses for study and vaccine testing easier. For his work, Enders and his team won the Nobel prize in physiology or medicine.
In 1951, Jonas Salk’s team from Pittsburgh produced a method to culture poliovirus in monkey kidney tissue. This allowed for large-scale virus production to make a killed-virus vaccine. Early trials showed success and the Salk team was allowed to do large-scale testing with Thomas Francis. When the results arrived in 1955, Francis announced to the world that Salk vaccine was seventy percent effective against the most prevalent strain of poliovirus, and ninety percent effective against the other, less common strains. The trial tested more than two million children among which around a million were in the control group. The same day the US government licensed the vaccine for widespread distribution and use. This monumental success made Jonas Salk famous all over the world. The US launched mass vaccination programs reducing polio cases from 30000 a year to 161 in 1961.
Everyone was not on the same page as Salk. Albert Sabin and Hilary Koprowski disagreed with Salk’s killed-virus vaccine approach. They thought it produced a weaker response and needed more doses of the vaccine than the attenuated vaccine. Also, the Salk vaccine did not protect against infection in the intestine. In 1948 Hilary Koprowski at Lederle labs developed an attenuated type II poliovirus vaccine, which he and his assistant drank. They suffered no side effects, demonstrating the world’s first effective live polio vaccine. Sabin also successfully managed to produce an oral vaccine based on attenuated mutants of poliovirus in 1954. Sabin and Koprowski could not test their vaccine because of the US government’s massive Salk vaccine campaign.
Coincidently Mikhail Chumakov and some other Soviet virologists were visiting the US to study the Salk vaccine in 1956. In Cincinnati, they met Sabin. Sabin was born in Russia and spoke a little Russian; Chumakov and Sabin became friends instantly. The Soviet delegation invited Sabin and Salk to visit the USSR. Salk refused. Sabin, after interrogation by the FBI, managed to go to the USSR amid cold war tensions and begin the collaboration which would bring the oral vaccine to light. Sabin did the testing in the USSR and Mexico, and Koprowski did it in Congo and Poland.
In 1958-1959 Chumakov organized the first mass production and clinical trials of Oral Poliovirus Vaccine (OPV), a cheaper alternative to the Salk vaccine. It was administered with a drop or on a sugar cube. The USSR produced this highly effective vaccine and exported it to more than 60 countries, which stopped large outbreaks in Russia, Eastern Europe, and Japan. The US administration was skeptical earlier of Sabin’s communist vaccine, but they licensed it in 1962. Sabin’s vaccine became the main tool used in the global poliomyelitis eradication campaign.
Nanos gigantium humeris insidentes
In the early twentieth century, there were tons of diseases going around the world without a vaccine, like measles, chickenpox, mums. Techniques for vaccination developed by Edward Jenner and Louis Pasteur were pushed further by Jonas Salk, Albert Sabin, and researchers all over the world. Progress in basic biology, chemistry, physics, and engineering helped to move this vaccine research forward. Tissue and bacteria culture helped in understanding the viruses; polymer science and industrial filters helped in isolating viruses and related proteins; optics and quantum physics helped in imaging these pathogens. One tends to rush in giving credit to an individual person, organization, or country for developments in science, but science does not work this way; like Newton once said, “If I have seen further, it is by standing on the shoulders of giants.” Indeed, scientists across disciplines and decades collaborate in unimaginable ways to produce the wonderful things in the world.
Vaccination campaigns and Impact
Fortunately, neither Salk nor Sabin patented their vaccine and gave it away to the governments around the world. Salk gave a television interview to Edward Murrow, who asked him, “Who owns the patent on this vaccine?” “The people,” Salk said, nobly. “There is no patent. Could you patent the sun?” World Health Organization and United Nation led efforts with OPV from USSR to eradicate polio from the world. One could recall the Pulse polio campaign from 1994 by the Indian government in collaboration with UNICEF, WHO (World Health Organization), and international charities. It was a tremendous achievement in public awareness of the disease and community vaccination. Around 174 million children under 5 years of age are given polio drops in these drives. In 2014, India was declared polio-free by WHO.
Profit over people
In the world we inhabit, profits drive the production of medical necessities. Even lifesaving drugs and vaccines are subject to market risks and intellectual property protections. Forbes magazine analysis from 2012 suggests that Salk would have been 7 billion USD richer if he had patented the vaccine. One needs to take a hard look at the production of vaccines in today’s world. The basic research for most of the vaccines happens in public institutions, which is taken over by pharmaceutical companies for large-scale manufacturing. In India, previously vaccine production was done by many government-owned companies for massive immunisation drives for children. However, in recent decades, several private companies have grown rapidly compared to public vaccine manufacturers. This could be blamed on lack of public funding, privatization, or globalisation. Currently, India is one of the largest manufacturers and exporters of vaccines, but it also has one of the highest rates of vaccine-preventable diseases in the world. Though polio has been eradicated from India, close to 2 million lives are lost every year due to these other diseases.
While the coronavirus wreaking havoc on Indian society, only two companies, Serum Institute and Bharat Biotech, are allowed to make vaccines while state-owned vaccine manufacturers sit idle. The shortage of vaccines and lack of immunisations could be attributed to several factors, like lack of cold chain infrastructure, minimal resource allocation by the government, or inaccessible technology. By ‘inaccessible technology’, I mean that global trade relationships put a price tag on state-of-the-art technology for some oligarchical companies to make enormous amounts of profit. This is enforced by organisations like World Trade Organization and International Monetary Fund. Trade-Related Aspects of Intellectual Property Rights (TRIPS) Agreement is one of their instruments, where intellectual property of few big companies in developed countries is protected making underdeveloped countries dependent on them. Currently, India and South Africa have put forth a resolution to waive patent rights on the Covid vaccines, so that the idle pharmaceutical companies all over the world could manufacture it. This is still under consideration, and indecisiveness on this waiver has costed lives. All in the name of profit incentive for innovation of the transnational corporations.
Last year India added 40 new billionaires to the ever-growing list. Business Standard reports “It’s raining billionaires in India’s pharma and health care space.” We should question the current system where few make millions of dollars, and millions suffer consequences of deadly diseases. The latest news says that the Bharat biotech vaccine might be licensed to other companies for scaling up production. It still does not compare to the poliovirus vaccine, where vaccines were developed with public funding, and the best vaccine was produced at a wide scale to save millions of children. The story of the polio vaccine is a story of global scientific cooperation in face of a health emergency. Also, it is a reminder to all of us, how important basic science discoveries are to the development of complex technologies as vaccines. Short term profit-oriented corporations would not have foresight for developing science. We need people-oriented science for society. As John Donne’s poem goes, “No man is an island entire of itself; every man is a piece of the continent, a part of the main.” No science is complete by itself but is complemented by humanity. Emancipating science from profit motive is the only solution for the future benefit of humankind.
Sources and further readings:
- indecisiveness-on-trips-waiver-cost-2-million-lives-india-to-wto-9503981.htm
- https://economictimes.indiatimes.com/industry
- vaccine-market-in-india-opportunities-for-dutch-vaccine-industry.pdf
- state-owned-vaccine-manufacturers-sit-idle-as-india-scours-for-jabs-report
- https://thewire.in/health/india-leads-in-vaccine-production-but-not-in-vaccination
- https://www.thehindu.com/sci-tech/health/what-is-pulse-polio/article22645159.ece
- https://hekint.org/2020/05/11/a-cold-war-vaccine-albert-sabin-russia-and-the-oral-polio-vaccine/
- https://www.scientificamerican.com/article/birth-of-a-cold-war-vaccine/
- https://www.newyorker.com/science/annals-of-medicine/the-last-time-a-vaccine-saved-america
- https://www.historyofvaccines.org/timeline#EVT_100326
- David M. Oshinsky, Polio: An American Story, Oxford University Press, 2005
- CDC report
- https://www.nytimes.com/2021/02/23/business/covid-vaccine-monkeys.html
- https://www.thelancet.com/journals/lancet/article/PIIS0140-67360416746-9/fulltext
- https://inequality.org/great-divide/dr-billionaire-meet-dr-salk/
- https://www.pbs.org/wgbh/aso/databank/entries/dm52sa.html
- https://louisproyect.org/2020/03/14/polio-covid-19-and-socialism/
- https://spectrejournal.com/turning-a-profit-from-death/
- https://www.aljazeera.com/opinions/2021/2/21/the-vaccine-debacle-shows-the-predatory-nature-of-capitalism
Originally written for Breakthrough Science Society Abroad Magazine